RESOURCES
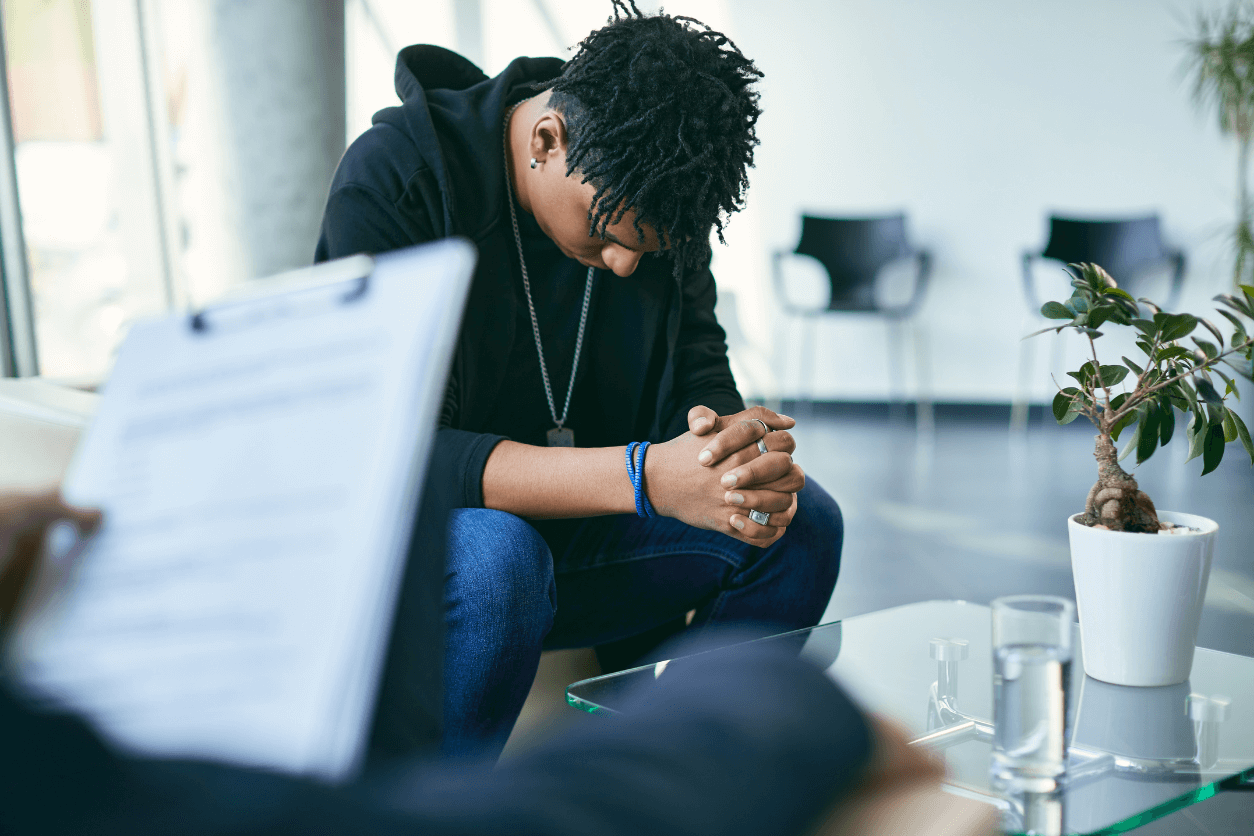
If we want a brighter future for mental health and substance use, it will take all of us doing our part.
Below are some of our resources to help organizations of all types ensure mental healthcare and substance use treatment are part of their plan forward.
Clinicians
Empowering front-line primary care physicians who see the most cases of mental illness and prescribe the most psychotropic drugs—including pediatrics, geriatric, ObGyns, and family doctors. Also, training both psychiatrists and behavioral health coordinators (bachelor’s or associate’s degree) who, together with primary care providers, make up the care team.

Jul 17, 2024
ResourceIntegrating Behavioral Health Care into Primary Care Settings: The Collaborative Care Model
The Collaborative Care Model: How it works, how it can be integrated into primary and specialty care settings, and its many benefits.

Jun 16, 2023
ResourceUsing the Collaborative Care Model for Special Populations
The learning modules provided by the APA include resources and guidance on how the CoCM can be used to treat specific populations. Practices have successfully adapted and implemented the CoCM to deliver mental health care to the following special patient populations: Geriatric, Pediatric, Perinatal, and Substance Use Disorders.

Nov 23, 2022
ResourceCollaborative Care Model 101
From our partner organization, the American Psychiatric Association, these resources explain the Collaborative Care Model and how to successfully integrate it into a primary care setting, including training, implementation, reimbursement, and more.

May 16, 2022
ResourceThe Practice and Billing Toolkit: Tools for successful implementation of the Collaborative Care Model
The American Psychiatric Association created a toolkit compiling sample tools and resources from pioneer practices that have implemented the Collaborative Care Model (CoCM) and are billing for services delivered in the model.
Health Systems
Equipping entire health systems in the United States to detect and treat mental illness in its early stages and to better serve all patients—especially adolescents and transition-age youth.

Feb 27, 2024
ArticleMeadows Mental Health Policy Institute Shares Results of its Novel Study on the Collaborative Care Model
This report explains how the Collaborative Care Model can potentially mitigate mental healthcare accessibility and the healthcare workforce shortage by providing effective and financially sustainable care to patients on a large scale.

Nov 1, 2023
EventAPA’s 2023 Mental Health Conference Features Discussion of Pediatric Collaborative Care Model
The 2023 Mental Health Services Conference of the American Psychiatric Association featured a discussion of the pediatric Collaborative Care Model that was led by a team from the Meadows Institute.


Apr 17, 2023
ReportImproving Behavioral Health Care for Youth Through Collaborative Care Expansion
The Collaborative Care Model (CoCM) stands out as the most evidence-based method for integrating behavioral health into primary care. Despite its proven effectiveness, especially for children and adolescents, adoption has been slow, particularly in pediatric practices.


Apr 1, 2023
ReportCollaborative Care Implementation Costs Across Health Care Systems
Report analyzing CoCM implementation cost data from 10 health systems nationwide that varied in size, U.S. region, and urban or rural setting.


Mar 17, 2022
ReportIntegration and the Pediatric Behavioral Health Workforce
Integrating mental health and substance use treatment into pediatric care holds tremendous potential for addressing workforce challenges. By leveraging both pediatric primary care and behavioral health specialty care workforces, we can make significant strides in providing comprehensive care to young patients.
Employers
Giving purchasers of all kinds—employers, unions, and states—the tools they need to make adjustments to how they negotiate with insurance carriers. Download Our Full Checklist.


Jun 10, 2024
ReportThe Path to National Leadership: The First Business-Led Statewide Mental Health Initiative
The first business-led statewide mental health initiative is here! Launched at the 2024 Leadership Conference on Safety and Sustainability, headlined by Michael Phelps, the initiative focuses on making Florida a top-five state for overall well-being and, ultimately, the healthiest state in America.

Jan 17, 2024
ResourceEngaging Insurers on Behavioral Health – An Employer Resource
The issues of mental health access and quality have become increasingly recognized as foundational to employer health strategy.
Key Focus Areas: Network Access, Other Access, Quality of Care Management, Integration into Primary Care and Workplace Mental Health.

Oct 10, 2023
ReportImproving Network Adequacy for Mental Health Care and Substance Use Disorders
The Path Forward Coalition has released a new report: “Equitable Access to Care for Mental Health and Substance Use Disorders: Standards, Measures, and Enforcement of Network Adequacy.”

Sep 17, 2023
ResourceEmployer Action Plan
Take charge of mental health care for millions of Americans with the purchasing power in your hands. What it takes is a just a few small changes to how purchasers negotiate with insurance companies and third-party administrators. And we are here to help.

Dec 17, 2022
ResourceAdvanced Request for Information: Behavioral Health Integration
This Advanced Primary Care RFI builds off the principles outlined in the PBGH Common Purchasing Agreement and is intended to be used by purchasers interested in making advanced primary care available for their employees.

Mar 20, 2022
TestimonyUS Senate, Finance Committee Hearing on Behavioral Health Care When Americans Need It
HR Policy statement to the Senate Finance Committee recommending any legislation include funding for integrated care, specifically the Collaborative Care Model, and remove barriers employers face in expanding telehealth offerings to employees.
Insurers
Empowering insurers to scale the Collaborative Care Model through investment in training and startup costs.
May 18, 2024
EventRecap: Mid-Atlantic Path Forward Webinar on the Collaborative Care Model
This webinar delved into the intricate implementation of the Collaborative Care Model within primary care settings. Attendees gained valuable insights into how these programs are being integrated, the progress they have made, and their current status.

Sep 29, 2023
ResourceMental Health Association of Maryland Host Second Webinar on Collaborative Care Model
The webinar series serves as a platform for healthcare professionals, policymakers, and stakeholders to share their experiences and learn from each other’s successes and challenges in adopting the Collaborative Care Model.

May 17, 2023
Case StudyBlue Cross Blue Shield of Michigan’s Collaborative Care Model Improves Patient Health and Lowers Costs
Studies show that chronic conditions can be better managed when behavioral health problems are addressed. Patients get better faster. And care costs less.


Jan 1, 2022
ReportCollaborative Care Implementation Costs Across Health Care Systems
This report from MMHPI analyzes CoCM implementation cost data from 10 health systems nationwide that varied in size, U.S. region, and urban or rural setting.
