Collaborative Care Model 101
From our partner organization the American Psychiatric Association.
The Collaborative Care Model for Mental Health: Improves Outcomes, Reduces Costs
Issue: One in five Americans experienced mental illness in the past year.1 Mental health and substance use disorders (MH/SUD) are often chronic conditions that people experience with other health conditions, such as heart disease and diabetes. Yet, only 25 percent of patients receive effective mental health care, including in primary care settings, where the majority of patients with MH/SUD receive their usual care.2
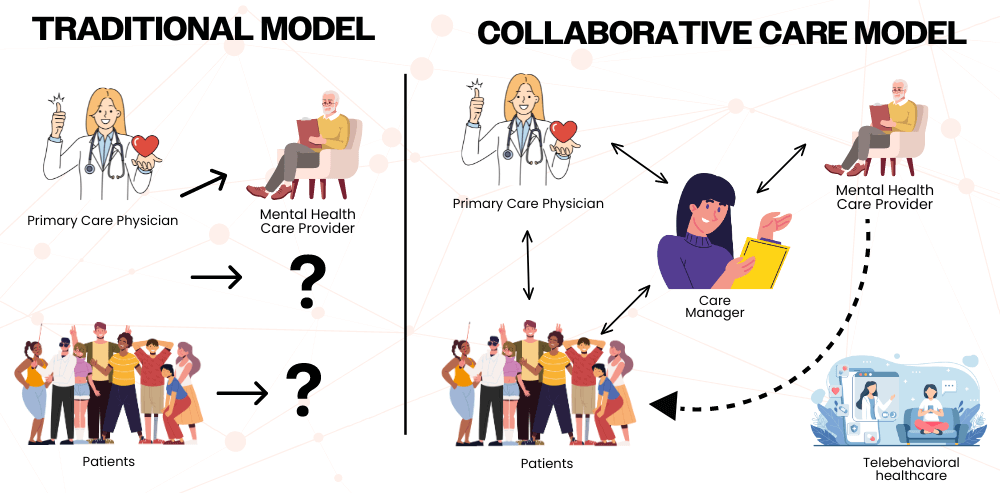
A Solution: Better care coordination via integration of mental health and primary care has been shown to improve patient access and outcomes. Three decades of research and over 80 randomized controlled trials (RCT) have identified one model in particular – the Collaborative Care Model (CoCM) – as being effective and efficient in delivering integrated care.3 It is estimated that $26 – $48 billion could be saved annually through effective integration of mental health and other medical care.4 The CoCM uses a team-based, interdisciplinary approach to deliver evidence-based diagnoses, treatment and follow-up care. The CoCM can be adapted to small and large, and rural and urban primary care practices.
3 Core Elements Make Up the CoCM
- Care coordination and care management by a social worker or psychologist, working with the primary care provider (PCP),
- Regular, proactive outcome monitoring and treatment to a specific outcomes target using standardized outcome measures/rating scales and utilizing electronic tools, such as patient tracking, and
- Regular, systematic psychiatric caseload reviews in person or through telemedicine with a psychiatrist, or nurse practitioner/physician assistant with psychiatric training, whose primary responsibilities are making treatment recommendations.
However, successfully expanding use of the model will depend on the availability of reimbursement for services related to care management and psychiatric consultation, and infrastructure support for staffing changes and implementation of data tracking tools. The Centers for Medicare and Medicaid Services approved reimbursement codes for the model in its 2017 Medicare Physician Fee Schedule (PFS). The CY 2018 Final Rule released updated payment policies, payment rates, and other provisions for services furnished under the Medicare PFS on or after Jan. 1, 2018. To date, CoCM services have typically been covered by grants.
Recommendations
• Support coverage and reimbursement for the CoCM as approved in the 2017 Medicare Physician Fee Schedule.
Additional Resources from APA
1 – Department of Health and Human Services. “Mental Health Myths and Facts.” http://www.mentalhealth.gov/basics/myths-facts/
2 – Unützer J et al. “The Collaborative Care Model: An Approach for Integrating Physical and Mental Health Care in Medicaid Health Homes.” Health Home Information Resource Center Brief. Centers for Medicare and Medicaid Services. May 2013.
3 – Advancing Integrated Mental Health Solutions (AIMS) Center. “Evidence Base.” https://aims.uw.edu/collaborative-care/evidence-base
4- Milliman, Inc. “Economic Impact of Integrated Medical-Behavioral Healthcare. Implications for Psychiatry.” April 2014
