Collaborative Care Heat Map
Collaborative Care: Gains, Gaps and Opportunities
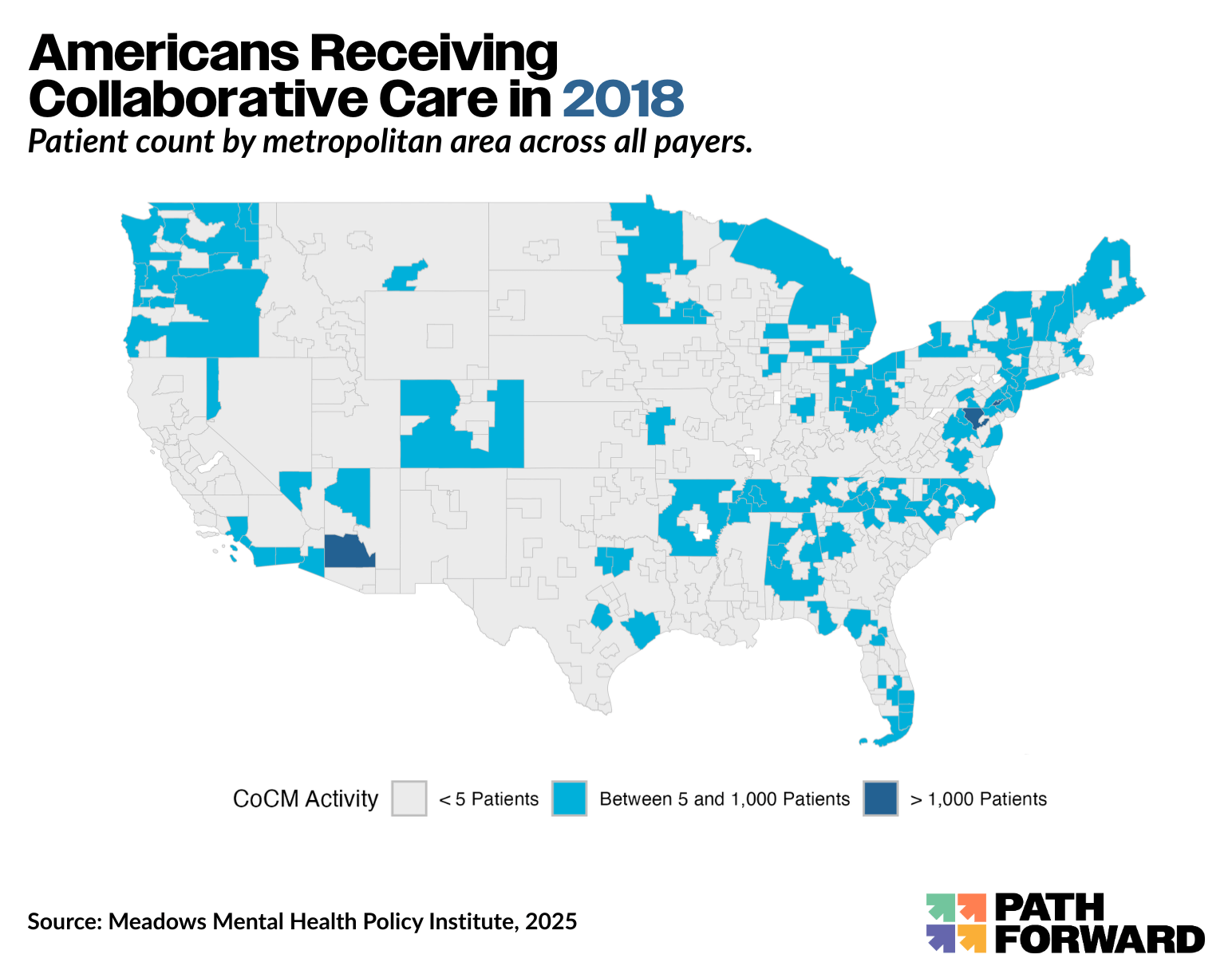
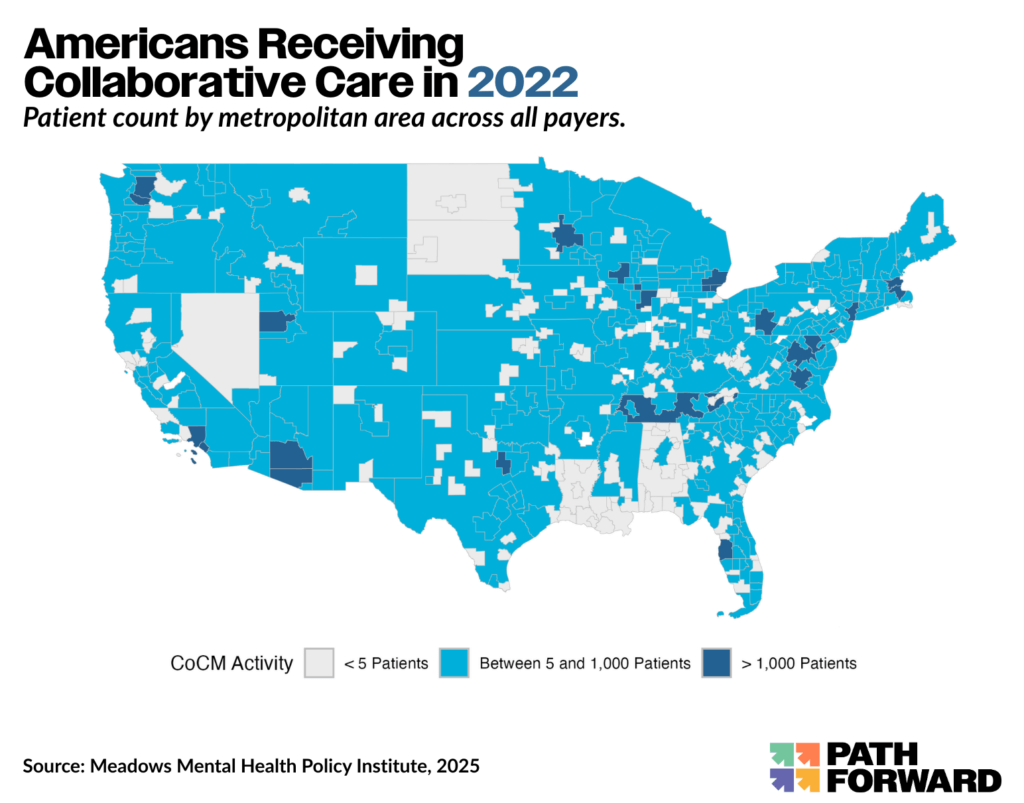
The map below was developed by the Meadows Mental Health Policy Institute, on behalf of Path Forward, and in partnership with the American Psychiatric Association. Based on data analyzed by Milliman, it represents the experience of 219 million Americans. This powerful tool, designed for policymakers, payers, and providers, supports strategic, data-informed expansion. This work was made possible through the support of The Goodness Web and West Health.
About Collaborative Care
What is Collaborative Care?
The Collaborative Care Model is an integrated approach to treating common mental health conditions like depression and anxiety within primary care settings. It brings together a team of health professionals—typically a primary care provider, a behavioral health care manager, and a psychiatric consultant—who work together to provide coordinated, measurement-based care. This model allows patients to receive mental health support in the same place they get their regular medical care, improving access, continuity, and overall outcomes.
A Proven, Scalable, Sustainable Model
Collaborative Care is one of the most rigorously studied models of behavioral health integration. More than 90 randomized controlled trials have demonstrated its effectiveness in improving mental health outcomes, reducing symptoms, and improving recovery rates—particularly for depression and anxiety. Collaborative Care, if implemented nationwide, could save 14K lives from suicide. It reduces remission time for depression 7X, leverages psychiatrists’ time to reach 8X more patients, and is 100% self-sustaining once startup hurdles are overcome.
Milliman Report
This Milliman analysis highlights where the Collaborative Care Model is being used—and where it’s missing.
The analysis, reflecting the experience of 219 million Americans, was commissioned by the Meadows Mental Health Policy Institute on behalf of Path Forward and in partnership with the American Psychiatric Association.
Key Findings
Explore the story behind the data.
Scroll through the visualizations below to see some of the key findings from the Milliman analysis. These snapshots offer a high-level look at trends in Collaborative Care adoption across the U.S. For deeper insights, including regional breakdowns and methodology, see the full report and appendices.
Note: All rates shown are unadjusted and may reflect underlying differences in population characteristics.
Partner Resources
Our partners—the American Psychiatric Association and Meadows Mental Health Policy Institute—offer a robust collection of tools to support the implementation of Collaborative Care across a variety of clinical settings. From practical guides and financial modeling tools to training programs and policy resources, their materials are designed to help providers, payers, employers, and advocates take action.
Explore the resources below to find what’s most relevant to your role in advancing integrated mental health care.
American Psychiatric Association
Meadows Mental Health Policy Insitute
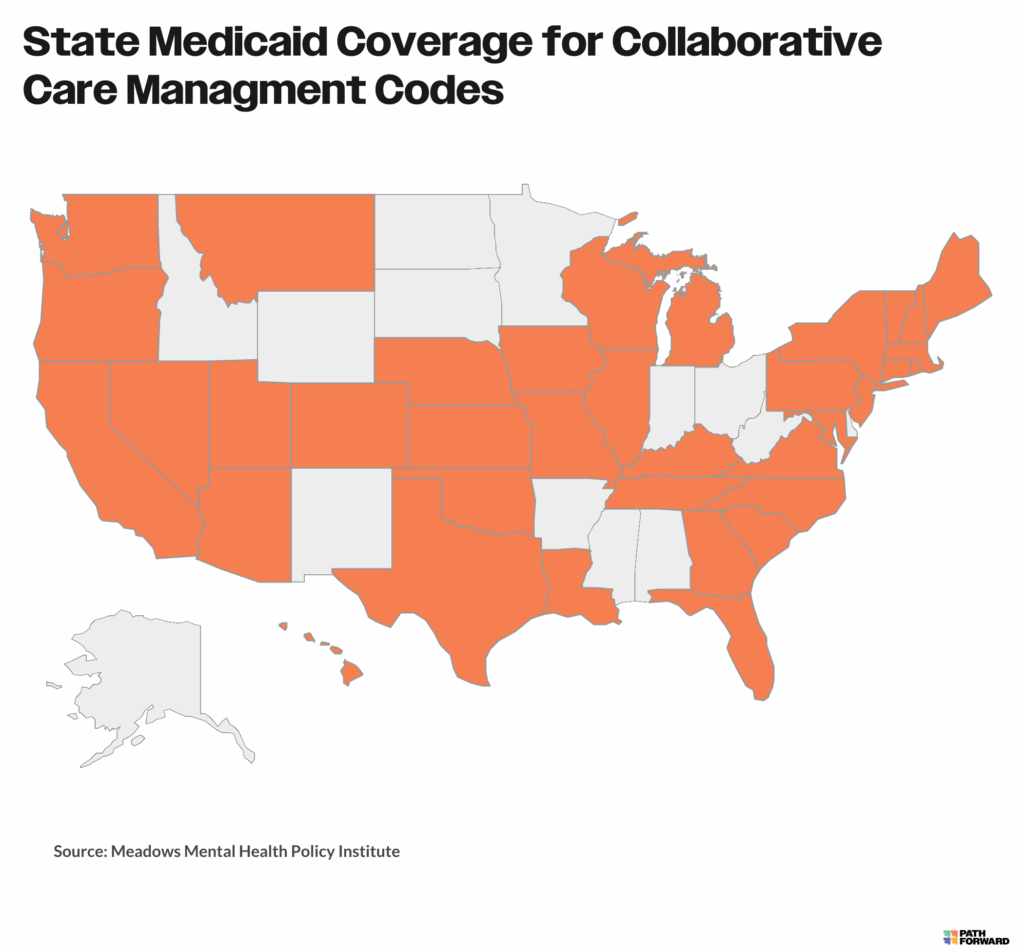
This resource offers a clear snapshot of how state Medicaid programs are adopting the Collaborative Care Management (CoCM) billing codes (99492–99494 and G2214).
You’ll find:
-
Which states currently cover CoCM codes under Medicaid
-
Reimbursement rates listed in state Medicaid fee schedules
-
How Medicaid and Medicare reimbursement rates compare, by state
-
Any state-specific restrictions or requirements for billing
The information is drawn from a thorough review of public Medicaid policies and guidance. While it’s a helpful starting point, we recommend checking directly with state Medicaid agencies or managed care organizations to confirm the most up-to-date details.
Family Medicine Centers
The Meadows Mental Health Policy Institute (MMHPI) technical assistance (TA) team partnered with Family Medicine Centers (FMC) successfully launched a full-scale Collaborative Care (CoCM) program, bringing mental health services into primary care.
This effort has expanded access to affordable, effective behavioral health care for hundreds of patients across the Texas Panhandle—a largely rural area with limited mental health resources. FMC’s leadership and commitment were key to making CoCM work in their clinics and improving care for their community.
Baylor Scott & White Health
The Meadows Mental Health Policy Institute (MMHPI) worked with Baylor Scott & White Health (BSW) to bring Collaborative Care (CoCM) to their Family and Internal Medicine Clinics across Central and North Texas.
With MMHPI’s support, BSW successfully integrated mental health care into primary care settings, improving access to affordable, effective treatment for more than 7,000 patients facing common behavioral health challenges.
Texas A & M
With support from the Meadows Mental Health Policy Institute (MMHPI), Texas A&M University Health Services (UHS) brought Collaborative Care (CoCM) into their student health clinic—integrating mental health into primary care for their student population.
This initiative has expanded access to affordable, effective care for more than 77,000 students. Texas A&M is among the first universities in the nation to offer CoCM through student health services, setting a powerful example for campus-based mental health care.
The Meadows Institute, in collaboration with key partners, created a set of practical tools to help care teams successfully implement high-quality Collaborative Care (CoCM).
These resources are designed to support real-world adoption and ensure programs are delivered with fidelity to the model.
Collaborative Care (CoCM) is one of the most well-studied and proven approaches to integrating mental health care into primary care. Its effectiveness has been backed by more than 90 randomized controlled trials and several meta-analyses across a wide range of conditions—including depression, anxiety, and bipolar disorder—as well as across diverse populations like older adults and people with chronic medical conditions. It works in a variety of care settings, from community health centers to the VA.
CoCM has also been shown to help close gaps in care, reducing racial and ethnic disparities in mental health outcomes. It’s a strong option for rural and underserved communities, and it’s supported by designated billing codes that are reimbursed by Medicare, most commercial insurers, and a growing number of state Medicaid programs—making it a financially viable model.
Below, you’ll find research, reviews, and real-world studies that highlight the strength and impact of Collaborative Care.